Services
-
 Braces / Invisalign
Braces / Invisalign
-
 Bridges & Crowns
Bridges & Crowns
-
 Tooth Extraction
Tooth Extraction
-
 Dental Implants
Dental Implants
-
 Dentures
Dentures
-
 Root Canal Treatment
Root Canal Treatment
-
 Teeth Whitening
Teeth Whitening

BRACES/ INVISALIGN
Clear aligners, also known as clear-aligner treatment, are orthodontic devices that are a transparent, plastic form of dental braces used to adjust teeth. As of 2017, there are more than 27 products available including ClearCorrect and Invisalign.
Clear aligners have undergone changes, making assessment of effectiveness difficult. A 2014 systematic review concluded that published studies were of insufficient quality to determine effectiveness. Experience suggests they are effective for moderate crowding of the front teeth, but less effective than conventional braces for several other issues and are not recommended for children. In particular they are indicated for “mild to moderate crowding (1–6 mm) and mild to moderate spacing (1–6 mm)”, in cases where there are no discrepancies of the jawbone. They are also indicated for patients who have experienced a relapse after fixed orthodontic treatment.
Clear-aligner treatment involves an orthodontist or dentist, or with home-based systems, the person themselves, taking a mold of the patient’s teeth, which is used to create a digital tooth scan. The computerized model suggests stages between the current and desired teeth positions, and aligners are created for each stage. Each aligner is worn for 20 hours a day for two weeks. These slowly move the teeth into the position agreed between the orthodontist or dentist and the patient. The average treatment time is 13.5 months

BRIDGES& CROWNS
A bridge is a fixed dental restoration (a fixed dental prosthesis) used to replace one or more missing teeth by joining an artificial tooth definitively to adjacent teeth or dental implants.
Definitions
Fixed bridge: A dental prosthesis that is definitively attached to natural teeth and replaces missing teeth.
Abutment: The tooth that supports and retains a dental prosthesis.
Pontic: The artificial tooth that replaces a missing natural tooth.
Retainer: The component attached to the abutment for retention of the prosthesis. Retainers can be major or minor.
Unit: Pontics and abutment teeth are referred to as units. The total number of units in a bridge is equal to the number of pontics plus the number of abutment teeth.
Saddle: The area on the alveolar ridge which is edentulous where at least one missing tooth is to be reinstated.
Connector: Joins the pontic to the retainer or two retainers together. Connectors may be fixed or movable.
Span: The length of the alveolar ridge between the natural teeth where the bridge will be placed.
Abutment: The tooth or implant that supports and retains a dental prosthesis.
Resin bonded bridge: A dental prostheses where the pontic is connected to the surface of natural teeth which are either unprepared or minimally prepared.

TOOTH EXTRACTION
A dental extraction (also referred to as tooth extraction, exodontia, exodontics, or informally, tooth pulling) is the removal of teeth from the dental alveolus (socket) in the alveolar bone. Extractions are performed for a wide variety of reasons, but most commonly to remove teeth which have become unrestorable through tooth decay, periodontal disease, or dental trauma, especially when they are associated with toothache. Sometimes wisdom teeth are impacted (stuck and unable to grow normally into the mouth) and may cause recurrent infections of the gum (pericoronitis). In orthodontics if the teeth are crowded, sound teeth may be extracted (often bicuspids) to create space so the rest of the teeth can be straightened.
Tooth extraction is usually relatively straightforward, and the vast majority can be usually performed quickly while the individual is awake by using local anesthetic injections to eliminate pain. While local anesthetic blocks pain, mechanical forces are still felt. Some teeth are more difficult to remove for several reasons, especially related to the tooth’s position, the shape of the tooth roots, and the integrity of the tooth. Dental phobia is an issue for some individuals, and tooth extraction tends to be feared more than other dental treatments such as fillings. If a tooth is buried in the bone, a surgical or trans alveolar approach may be required, which involves cutting the gum away and removing the bone which is holding the tooth in with a surgical drill. After the tooth is removed, stitches are used to replace the gum into the normal position.
Immediately after the tooth is removed, a bite pack is used to apply pressure to the tooth socket and stop the bleeding. After a tooth extraction, dentists usually give advice which revolves around not disturbing the blood clot in the socket by not touching the area with a finger or the tongue, by avoiding vigorous rinsing of the mouth, and avoiding strenuous activity. Sucking, such as through a straw, is to be avoided. If the blood clot is dislodged, bleeding can restart, or alveolar osteitis (“dry socket”) can develop, which can be very painful and lead to delayed healing of the socket. Smoking is avoided for at least 24 hours as it impairs wound healing and makes dry socket significantly more likely. Most advise hot salt water mouth baths which start 24 hours after the extraction.
The branch of dentistry that deals primarily with extractions is oral surgery (“exodontistry”), although general dentists and periodontists often carry out tooth extraction routinely since it is a core skill taught in dental schools. Periodontists are performing more and more extractions, since they often follow up and place a dental implant.
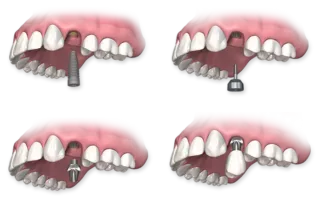
DENTAL IMPLANTS
The primary use of dental implants is to support dental prosthetics. Modern dental implants make use of osseointegration, the biologic process where bone fuses tightly to the surface of specific materials such as titanium and some ceramics. The integration of implant and bone can support physical loads for decades without failure.
For individual tooth replacement, an implant abutment is first secured to the implant with an abutment screw. A crown (the dental prosthesis) is then connected to the abutment with dental cement, a small screw, or fused with the abutment as one piece during fabrication. Dental implants, in the same way, can also be used to retain a multiple tooth dental prosthesis either in the form of a fixed bridge or removable dentures.
An implant supported bridge (or fixed denture) is a group of teeth secured to dental implants so the prosthetic cannot be removed by the user. Bridges typically connect to more than one implant and may also connect to teeth as anchor points. Typically the number of teeth will outnumber the anchor points with the teeth that are directly over the implants referred to as abutments and those between abutments referred to as pontics. Implant supported bridges attach to implant abutments in the same way as a single tooth implant replacement. A fixed bridge may replace as few as two teeth (also known as a fixed partial denture) and may extend to replace an entire arch of teeth (also known as a fixed full denture). In both cases, the prosthesis is said to be fixed because it cannot be removed by the denture wearer.
A removable implant supported denture (also an implant supported overdenture. is a type of dental prosthesis which is not permanently fixed in place. The dental prosthesis can be disconnected from the implant abutments with finger pressure by the wearer. To enable this, the abutment is shaped as a small connector (a button, ball, bar or magnet) which can be connected to analogous adapters in the underside of the dental prosthesis. Facial prosthetics, used to correct facial deformities (e.g. from cancer treatment or injuries) can use connections to implants placed in the facial bones. Depending on the situation the implant may be used to retain either a fixed or removable prosthetic that replaces part of the face.[11]
In orthodontics, small diameter dental implants, referred to as Temporary Anchorage Devices (or TADs) can assist tooth movement by creating anchor points from which forces can be generated. For teeth to move, a force must be applied to them in the direction of the desired movement. The force stimulates cells in the periodontal ligament to cause bone remodeling, removing bone in the direction of travel of the tooth and adding it to the space created. In order to generate a force on a tooth, an anchor point (something that will not move) is needed. Since implants do not have a periodontal ligament, and bone remodelling will not be stimulated when tension is applied, they are ideal anchor points in orthodontics. Typically, implants designed for orthodontic movement are small and do not fully osseointegrate, allowing easy removal following treatment.

DENTURES
Dentures (also known as false teeth) are prosthetic devices constructed to replace missing teeth, and are supported by the surrounding soft and hard tissues of the oral cavity. Conventional dentures are removable (removable partial denture or complete denture). However, there are many denture designs, some which rely on bonding or clasping onto teeth or dental implants (fixed prosthodontics). There are two main categories of dentures, the distinction being whether they are used to replace missing teeth on the mandibular arch or on the maxillary arch.
Types
Removable partial dentures
Removable partial dentures are for patients who are missing some of their teeth on a particular arch. Fixed partial dentures, also known as “crown and bridge” dentures, are made from crowns that are fitted on the remaining teeth. They act as abutments and pontics and are made from materials resembling the missing teeth. Fixed bridges are more expensive than removable appliances but are more stable.
Another option in this category is the flexible partial, which takes advantage of innovations in digital technology. Flexible partial fabrication involves only non-invasive procedures. Dentures can be difficult to clean and can affect oral hygiene.
Complete dentures
Complete dentures are worn by patients who are missing all of the teeth in a single arch—i.e., the maxillary (upper) or mandibular (lower) arch—or, more commonly, in both arches.
Copy dentures
Can be made for either partial but mainly complete denture patients. These dentures require fewer visits to make and usually are made for older patients, patients who would have difficulty adjusting to new dentures, would like a spare pair of dentures or like the aesthetics of their dentures already. This requires taking an impression of the patients current denture and remaking them.
Materials
Dentures are mainly made from acrylic due to the ease of material manipulation and likeness to intra-oral tissues, ie. gums. Most dentures made are fabricated from heat-cured acrylic polymethyl methacrylate and rubber-reinforced polymethyl methacrylate. Coloring agents and synthetic fibers are added to obtain the tissue-like shade, and to mimic the small capillaries of the oral mucosa, respectively. However, dentures made from acrylic can be fragile and fracture easily if the patient has trouble adapting neuromuscular control. This can be overcome by reinforcing the denture base with cobalt chromium (Co-Cr). They are often thinner (therefore more comfortable) and stronger (to prevent repeating fractures).
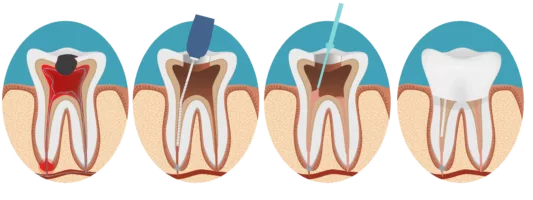
Root Canal Treatment
Root canal treatment (also known as endodontic therapy, endodontic treatment, or root canal therapy) is a treatment sequence for the infected pulp of a tooth which results in the elimination of infection and the protection of the decontaminated tooth from future microbial invasion. Root canals, and their associated pulp chamber, are the physical hollows within a tooth that are naturally inhabited by nerve tissue, blood vessels and other cellular entities. Together, these items constitute the dental pulp.
Endodontic therapy involves the removal of these structures, the subsequent shaping, cleaning, and decontamination of the hollows with small files and irrigating solutions, and the obturation (filling) of the decontaminated canals. Filling of the cleaned and decontaminated canals is done with an inert filling such as gutta-percha and typically a eugenol-based cement. Epoxy resin is employed to bind gutta-percha in some root canal procedures. Endodontics includes both primary and secondary endodontic treatments as well as periradicular surgery which is generally used for teeth that still have potential for salvage

TEETH WHITENING
The combination of intrinsic colour and the presence of extrinsic stains on the tooth surface influence the colour and thus the overall appearance of teeth. The scattering of light and absorption within enamel and dentine determine the intrinsic colour of teeth and because the enamel is relatively translucent, the dentinal properties can play a major role in determining the overall tooth colour. On the other hand, extrinsic stain and colour is the result of coloured regions that have formed within the acquired pellicle on the enamel surface and can be influenced by lifestyle behaviours or habits. For example, dietary intake of tannin-rich foods, poor tooth brushing technique, tobacco products, and exposure to iron salts and chlorhexidine can affect the colour of a tooth.
With increasing age, teeth tend to be darker in shade. This can be attributed to secondary dentin formation and thinning of enamel due to tooth wear which contributes to a significant decrease in lightness and increase in yellowness. Tooth shade is not influenced by gender or race
For a fast, efficient way to brighten your smile, consider what professional teeth whitening can do for you.
People all around the world are dazzled by a bright smile. The problem with the color of teeth is that it changes with time. Associated with age, tooth discoloration is actually not a sign of aging. This is evidenced by the number of people in their twenties and thirties who are already struggling with dull, stained enamel.
The real causes of a dull smile are foods and beverages that we consume, sometimes on a daily basis. Most people have heard that beverages like tea, coffee, and red wine can diminish the brightness of the smile. We also know that smoking can cause teeth to turn yellow or brown over time. But how?
Staining occurs bit by bit, sometimes over years. When you eat a food, drink a beverage, or use tobacco products, tiny particles from those substances are deposited onto enamel, which contains thousands of microscopic pores, just like your skin. When these deposits settle into enamel, they often remain for life – or until they can be lifted.
Professional teeth whitening has been perfected over hundreds of years of development. At Great Smiles Dental, we offer several different whitening treatments to meet the needs of our diverse patient base.
Tooth discolouration and staining is primarily due to two sources of stain: Extrinsic and Intrinsic.
Extrinsic staining
Extrinsic staining, is largely due to environmental factors including smoking, pigments in beverages and foods, antibiotics, and metals such as iron or copper. Coloured compounds from these sources are absorbed into acquired dental pellicle or directly onto the surface of the tooth causing a stain to appear.
- Dental plaque: Dental plaque is a clear biofilm of bacteria that naturally forms in the mouth, particularly along the gumline, and it occurs due to the normal development and defences of the immune system. Although usually virtually invisible on the tooth surface, plaque may become stained by chromogenic bacteria such as Actinomyces species. Prolonged dental plaque accumulation on the tooth surface can lead to enamel demineralisation and formation of white spot lesions which appear as an opaque milk-coloured lesion. The acidic by-products of fermentable carbohydrates derived from high-sugar foods contribute to greater proportions of bacteria, such as Streptococcus mutans and Lactobacillus in dental plaque. Higher consumption of fermentable carbohydrates will promote demineralisation and increase the risk of developing white spot lesions.
- Calculus: neglected plaque will eventually calcify, and lead to the formation of a hard deposit on the teeth, especially around the gumline. The organic matrix of dental plaque and calcified tissues undergo a series of chemical and morphological changes that lead to calcification of the dental plaque and therefore leading to the formation of calculus. The color of calculus varies, and may be grey, yellow, black, or brown. The colour of calculus depends on how long it has been present in the oral cavity for; it typically starts off yellow and over time the calculus will begin to stain a darker colour and become more tenacious and difficult to remove.
- Tobacco: tar in the smoke from tobacco products (and also smokeless tobacco products) tends to form a yellow-brown-black stain around the necks of the teeth above the gumline. The nicotine and tar in tobacco, combined with oxygen, turns yellow and over time will absorb into the pores of enamel and stain the teeth yellow. The dark brown to black stains along the gum line of the teeth are the result of the porous nature of calculus immediately picking up the stains from nicotine and tar.
- Betel chewing: Betel chewing produces blood-red saliva that stains the teeth red-brown to nearly black. The extract gel of betel leaf contain tannin, a chromogenic agent that causes discolouration of the tooth enamel.
- Tannin is also present in coffee, tea, and red wine and produces a chromogenic agent that can discolor teeth. Large consumption of tannin-containing beverages stain the dental enamel brown due to the chromogenic nature.
- Certain foods, including curries and tomato-based sauces, can cause teeth staining.
- Certain topical medications: Chlorhexidine (antiseptic mouthwash) binds to tannins, meaning that prolonged use in persons who consume coffee, tea or red wine is associated with extrinsic staining (i.e. removable staining) of teeth. Chlorhexidine mouthwash has a natural liking for sulphate and acidic groups commonly found in areas where plaque accumulates such as along the gumline, on the dorsum of the tongue and cavities. Chlorhexidine is retained in these areas and stain yellow-brown. The stains are not permanent and can be removed with proper brushing.
- Metallic compounds: Exposure to such metallic compounds may be in the form of medication or occupational exposure. Examples include iron (black stain), iodine (black), copper (green), nickel (green), and cadmium (yellow-brown). Sources of exposure to metal include placing metal into the oral cavity, metal containing dust inhalation, or oral administration of drugs. Metals can be penetrated into the tooth causing permanent discolouration or can bind to the pellicle causing surface stain.
Intrinsic staining
Intrinsic staining primarily occurs during the tooth development either before birth or at early childhood. Intrinsic stains are those that cannot be removed through mechanical measures such as debridement or a prophylactic stain removal. As the age of the person increases, the teeth can also appear yellower over time.Below are examples of intrinsic sources of stains:
- Tooth wear and ageing: Tooth wear is a progressive loss of enamel and dentine due to tooth erosion, abrasion and attrition. As enamel wears down, dentine becomes more apparent and chromogenic agents are penetrated in the tooth more easily. The natural production of secondary dentine also gradually darkens teeth with age.
- Dental caries (tooth decay): The evidence regarding carious tooth discolouration is inconclusive, however the most reliable evidence suggests that carious lesion allows for exogenous agents to enter dentine and hence increased absorption of chromogenic agents causing discolouration to the tooth.
- Restorative materials: The materials used during root canal treatments, such as eugenol and phenolic compounds, contain pigment that stain dentine. Restorations using amalgam also penetrate dentine tubules with tin over time therefore causing dark stains to the tooth.
- Dental trauma which may cause staining either as a result of pulp necrosis or internal resorption. Alternatively the tooth may become darker without pulp necrosis.
- Enamel hypoplasia: Enamel hypoplasia causes enamel to be thin and weak. It produces a yellow-brown discolouration and can also cause the enamel’s smooth surface to be rough and pitted which causes the tooth to be susceptible to extrinsic staining, tooth sensitivity, malocclusion, and dental caries. The evidence regarding enamel hypoplasia is inconclusive, however the most likely cause is infection or trauma caused to the primary dentition. Disturbances to the developing tooth germ during neonatal and early childhood stages such as maternal vitamin D deficiency, infection, and medication intake can cause enamel hypoplasia.
- Pulpal hyperemia: Pulpal hyperemia refers to inflammation of a traumatised tooth which can be caused by a stimuli such as trauma, thermal shock, or dental caries. Pulpal hyperemia is reversible and produces a red hue seen initially after trauma which has the ability to disappear if the tooth becomes revascularized.
- Fluorosis: Dental fluorosis causes enamel to become opaque, chalky white, and porous. The enamel can break down and cause the exposed subsurface enamel to become mottled and produce extrinsic dark brown-black stains. Dental fluorosis occurs due to excessive ingestion of fluoride or overexposure to fluoride during the development of enamel which usually occurs between the ages of one to four. Fluoridated drinking water, fluoride supplements, topical fluoride (fluoride toothpastes), and formula prescribed for children can increase the risk of dental fluorosis. Fluoride is considered an important factor in the management and prevention of dental caries, the safe level for daily fluoride intake is 0.05 to 0.07 mg/kg/day.
- Dentinogenesis imperfecta: Dentinogenesis imperfecta is a hereditary dentine defect, associated with osteogenesis imperfecta, which causes the tooth to become discoloured usually blue or brown in colour and translucent giving teeth an opalescent sheen. The condition is autosomal dominant which means that the condition runs in the family.
- Amelogenesis imperfecta: The appearance of amelogenesis imperfecta depends on the type of amelogenesis, there are 14 different subtypes and can vary from the appearance of hypoplasia to hypomineralisation which can produce different appearances of enamel from white mottling to yellow brown appearances.
- Tetracycline and minocycline: Tetracycline is a broad-spectrum antibiotic, and its derivative minocycline is common in the treatment of acne. The drug is able to chelate calcium ions and is incorporated into teeth, cartilage, and bone. Ingestion during the years of tooth development causes yellow-green discoloration of dentine visible through the enamel which is fluorescent under ultraviolet light. Later, the tetracycline is oxidized and the staining becomes more brown and no longer fluoresces under UV light.





